Risk Factors and Risk Assessment for Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis
By Chengjin Zhao, Ting Dai, Junbo Qian, Zhenming GeAffiliations
doi: 10.29271/jcpsp.2024.04.413ABSTRACT
Objective: To analyse the pertinent risk factors associated with post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP) and develop a predictive scoring system for assessing the risk of PEP in patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) procedures.
Study Design: Descriptive study.
Place and Duration of the Study: Department of Gastroenterology, Nantong First People's Hospital, Jiangsu, China, from January 2022 to January 2023.
Methodology: Clinical data of 375 patients who underwent successful ERCP treatment were collected and organised. Relevant risk factors for PEP were analysed, and a scoring system was established to predict the risk of PEP.
Results: Among the 375 patients who underwent ERCP, the incidence of PEP was 9.07% (34/375). Univariate analysis revealed that female gender, pancreatic duct opacification, difficult cannulation, operation time ≥45 minutes, sphincter of Oddi dysfunction (SOD), and biliary stenting were risk factors for PEP. Multivariate analysis showed that female gender, pancreatic duct opacification, difficult cannulation, operation time ≥45 minutes, and SOD were independent risk factors for PEP. A scoring system was developed, and the receiver operating characteristic (ROC) curve analysis determined a cut-off value of 1.5 points. Patients with a score less than 1.5 points had a low probability of developing PEP, while those with a score greater than 1.5 points had a significantly higher probability of PEP.
Conclusion: Female gender, pancreatic duct opacification, difficult cannulation, operation time ≥45 minutes, and SOD were independent risk factors for PEP. Additionally, a reliable scoring system was established to predict the risk of PEP. Clinicians can use this scoring system to assess the risk of PEP in patients and implement preventive measures to reduce the incidence of PEP.
Key Words: Endoscopic retrograde cholangiopancreatography, Post-ERCP pancreatitis, Risk factors, Risk assessment, Preventive measure.
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is an invasive procedure that has gained widespread use in the diagnosis and treatment of biliary and pancreatic diseases. Its advantages, including minimal trauma, fast recovery, and repeatability, have made it a commonly employed technique. Through sphincterotomy and stent placement, ERCP provides an effective and safe option for patients with bile or pancreatic duct obstruction. However, despite its benefits, ERCP can still give rise to certain complications, such as post-ERCP pancreatitis (PEP), postoperative biliary tract infection, gastrointestinal bleeding, gastrointestinal perforation, hypoxemia, cardiovascular accidents, and drug allergies.
PEP, in particular, is a serious and common complication, with an incidence rate ranging from approximately 5 to 15%,1 and even higher in high-risk populations, reaching 20 to 40%.2 While about 90% of PEP cases are mild, approximately 10% can progress to severe pancreatitis, resulting in prolonged hospitalisation, increased healthcare costs, and potential endangerment to the patient's life.3 The reported mortality rate in the literature ranges from 0.1 to 1.0%.4 Although previous studies have identified certain risk factors associated with PEP, further research is necessary to enhance the understanding and refine preventive measures.5 Additionally, most of the existing literature consists of international studies, and it is crucial to investigate the local patient population to determine the specific risk factors relevant to the region. In order to develop targeted preventive strategies, the rationale of this research was to contribute to the existing body of knowledge, improve the safety and effectiveness of ERCP procedures, and ultimately reduce the incidence of PEP. Additionally, the aim of the study was to analyse the incidence and risk factors associated with PEP and develop a scoring system to predict the likelihood of PEP occurrence.
METHODOLOGY
This retrospective study collected clinical data from patients who underwent ERCP at the Department of Gastroenterology, Nantong First People's Hospital, Nantong, China, between January 2022 and January 2023. A total of 375 patients were included in the study after applying predetermined inclusion and exclusion criteria. Access to patient records was obtained through the hospital information system (HIS), the hospital's electronic data system. Written informed consent was obtained from all patients and their family members who participated in the study.
Inclusion criteria for participant selection were patients who met the indications for ERCP, patients with normal serum amylase levels confirmed by pre-procedure testing, and inpatients with complete clinical information available. Exclusion criteria were severe cardiac, pulmonary, hepatic, or renal dysfunction that would hinder the procedure, pregnancy or lactation, known allergies to contrast agents, previous experience of bleeding or perforation during an ERCP procedure, acute pancreatitis or acute exacerbation of chronic pancreatitis, and mental disorders or non-compliance with treatment.
Preoperative preparations included routine laboratory tests, such as complete blood count, urinalysis, amylase, lipase, stool examination, liver and kidney function, and coagulation function. In addition, relevant imaging examinations, such as electrocardiogram, abdominal computed tomography (CT), or magnetic resonance cholangiopancreatography (MRCP), were conducted.
During the intraoperative phase, experienced endoscopists performed all procedures. Depending on the specific disease requirements, choledochography or pancreatic ductography was utilised to observe the lesion. Procedures including endoscopic sphincterotomy (EST), endoscopic papillary balloon dilatation (EPBD), mechanical lithotripsy, basket or balloon stone removal, biliary stent placement, pancreatic duct stent, and endoscopic nasobiliary drainage (ENBD) were performed as needed based on the patient's condition.
After surgery, patients were instructed to fast and rest in bed, while acid suppression drugs and fluid support therapy were administered. Venous blood samples were collected at 3, 6, and 24 hours postoperatively to measure serum amylase levels. If the amylase level did not show a significant increase within 24 hours after surgery, further testing was not required. However, if the level was elevated, additional blood samples were collected at 48 and 72 hours after surgery to monitor serum amylase levels. The amylase level was determined using a dry chemical method, with a normal range of 30-130 U/L.
Various patient factors were recorded, including gender, age, hypertension, diabetes, history of pancreatitis, history of ERCP, history of cholecystectomy, difficult cannulation (defined as an insertion time of ≥ 10 minutes or ≥5 insertion attempts), operation time, presence of pancreatic duct imaging, sphincter of Oddi dysfunction (SOD), presence of pancreatic duct stent, presence of duodenal diverticulum, and the use of nasobiliary drainage or biliary stent during ERCP. The risk scoring model assigned scores based on the rounded β values of five independent risk factors obtained from the logistic regression analysis. Specifically, female gender, pancreatic duct opacification, difficult cannulation, and operative time ≥45 minutes were each assigned 1 point, while SOD was assigned 2 points; otherwise, 0 points were assigned. The scores ranged from 0 to 6 points.
All factors potentially associated with PEP were analysed as risk factors using SPSS23.0 statistical software. Univariate and multivariate analyses were performed. Continuous variables were presented as mean ± standard deviation (SD), while categorical variables were presented as absolute numbers and percentages. Variables with a p-value ≤0.5 in the univariate logistic regression analysis were included in the multivariate logistic analysis to identify independent risk factors for PEP. A p-value < 0.05 was considered statistically significant. The independent risk factors identified were used to construct a risk assessment model, and the predictive value of the regression model was analysed using the receiver operating characteristic (ROC) curve.
RESULTS
During the period from January 2022 to January 2023, a total of 394 patients were scheduled to undergo ERCP surgery in Nantong First People's Hospital. Among these patients, 14 were excluded, including 8 cases of failed ERCP, 4 cases of bleeding and perforation complications, and 2 cases of contrast agent allergy. Eventually, 380 patients successfully underwent ERCP, but 5 of them were excluded from the study due to lost follow-up information as they were discharged early for further treatment at a community hospital. Therefore, a total of 375 patients were included in this study. Out of these, 34 cases developed PEP, resulting in an incidence rate of 9.07%. The mean age of all patients was 62.66 (SD ± 12.00) years. Among them, 190 (50.67%) were males and 185 (49.33%) were females. Detailed characteristics of all patients are presented in Table I.
In the univariate analysis, 16 parameters including age, gender, and hypertension were analysed. The results revealed significant differences (p <0.05) between the PEP and non-PEP groups in six variables including: gender (p = 0.012), SOD (p = 0.008), biliary stent placement (p = 0.044), difficult cannulation (p = 0.000), operation time ≥45 minutes (p = 0.001), and pancreatic duct opacification (p = 0.012, Table II).
For the multivariate analysis, PEP was used as the dependent variable, and the six variables with significant differences identified in the univariate analysis as well as nasobiliary drainage (p = 0.05) were used as independent variables. Gender (p = 0.012), SOD (p = 0.043), difficult cannulation (p = 0.033), operation time ≥45 minutes (p = 0.044), and pancreatic duct opacification (p = 0.003) were important independent risk factors for PEP (Table II).
Table I: Baseline characteristics of the patients.
|
Parameters |
Category |
Number |
PEP |
|
|
Yes (34) |
No (341) |
|||
|
Age |
<60 |
169 (45.1%) |
19 (11.2%) |
150 (88.8%) |
|
≥60 |
206 (54.9%) |
15 (7.3%) |
191 (92.7%) |
|
|
Gender |
Male |
190 (50.7%) |
10 (5.3%) |
180 (94.7%) |
|
Female |
185 (49.3%) |
24 (13.0%) |
161 (87.0%) |
|
|
Hypertension |
No |
257 (68.5%) |
22 (8.6%) |
235 (91.4%) |
|
Yes |
118 (31.5) |
12 (10.2%) |
106 (89.8%) |
|
|
Diabetes |
No |
318 (84.8%) |
29 (9.1%) |
289 (90.9%) |
|
Yes |
57 (15.2%) |
5 (8.8%) |
52 (91.2%) |
|
|
Previous ERCP |
No |
341 (90.9%) |
31 (9.1%) |
310 (90.9%) |
|
Yes |
34 (9.1%) |
3 (8.8%) |
31 (91.2%) |
|
|
Previous pancreatitis |
No |
331 (88.3%) |
30 (9.1%) |
301 (90.9%) |
|
Yes |
44 (11.7%) |
4 (9.1%) |
40 (90.9%) |
|
|
Previous cholecystectomy |
No |
253 (67.5) |
23 (9.1%) |
230 (90.9%) |
|
Yes |
122 (32.5%) |
11 (9.0%) |
111 (91.0%) |
|
|
SOD |
No |
368 (98.1%) |
30 (8.2%) |
338 (91.8%) |
|
Yes |
7 (1.9%) |
3 (42.9%) |
4 (57.1%) |
|
|
Duodenal diverticulum |
No |
320 (85.3%) |
27 (8.4%) |
293 (91.6%) |
|
Yes |
55 (14.7%) |
7 (12.7%) |
48 (87.3%) |
|
|
EST |
No |
35 (9.3%) |
5 (14.3%) |
30 (85.7%) |
|
Yes |
340 (90.7%) |
29 (8.5%) |
311 (91.5%) |
|
|
Difficult cannulation |
No |
297 (79.2%) |
18 (6.1%) |
279 (93.9%) |
|
Yes |
78 (20.8%) |
16 (20.5%) |
62 (79.5%) |
|
|
Operation time ≥45 min |
No |
311 (82.9%) |
21 (6.8%) |
290 (93.2%) |
|
Yes |
64 (17.1%) |
13 (20.3%) |
51 (79.7%) |
|
|
Pancreatic duct opacification |
No |
279 (74.4%) |
19 (6.8%) |
260 (93.2%) |
|
Yes |
96 (25.6%) |
15 (15.6%) |
81 (84.4%) |
|
|
Biliary stenting |
No |
276 (73.6%) |
20 (7.2%) |
256 (92.8%) |
|
Yes |
99 (26.4%) |
14 (14.1%) |
85 (85.9%) |
|
|
Nasobiliary drainage |
No |
91 (24.3%) |
13 (14.3%) |
78 (85.7%) |
|
Yes |
284 (75.7%) |
21 (7.4%) |
263 (92.6%) |
|
|
Bile duct dilation |
None |
167 (44.5%) |
19 (11.4%) |
148 (88.6%) |
|
M/M |
156 (41.6%) |
12 (7.7%) |
144 (92.3%) |
|
|
Sev |
52 (13.9%) |
3 (5.8%) |
49 (94.2%) |
|
|
PEP: Post-ERCP pancreatitis; ERCP: Endoscopic retrograde cholangiopancreatography; SOD: Sphincter of Oddi dysfunction; EST: Endoscopic sphincterotomy; M/M: Mild to moderate; Sev: Severe. |
||||
|
Variables |
Univariate analysis |
Multivariate analysis |
||||
|
OR |
95% CI |
p-value |
OR |
95% CI |
p-value |
|
|
Age ≥60 |
0.620 |
0.305-1.261 |
0.187 |
|
|
|
|
Female |
2.683 |
1.245-5.782 |
0.012* |
2.916 |
1.263-6.735 |
0.012* |
|
Hypertension |
1.209 |
0.577-2.534 |
0.615 |
|
|
|
|
Diabetes |
0.958 |
0.355-2.589 |
0.933 |
|
|
|
|
Previous ERCP |
0.968 |
0.280-3.348 |
0.959 |
|
|
|
|
Previous pancreatitis |
1.003 |
0.336-2.997 |
0.995 |
|
|
|
|
Previous cholecystectomy |
0.991 |
0.467-2.105 |
0.981 |
|
|
|
|
SOD |
8.153 |
1.745-38.088 |
0.008** |
7.699 |
1.062-52.820 |
0.043* |
|
Duodenal diverticulum |
1.583 |
0.653-3.837 |
0.310 |
|
|
|
|
Bile duct dilation |
|
|
|
|
|
|
|
None |
|
|
|
|
|
|
|
Mild-moderate |
2.040 |
0.579-7.195 |
0.267 |
|
|
|
|
Severe |
1.333 |
0.361-4.925 |
0.666 |
|
|
|
|
Biliary stenting |
2.108 |
1.020-4.356 |
0.044* |
0.929 |
0.191-4.505 |
0.927 |
|
Difficult cannulation |
4.000 |
1.932-8.279 |
0.000*** |
2.762 |
1.086-7.027 |
0.033* |
|
Operation time ≥45 minutes |
3.520 |
1.658-7.474 |
0.001** |
2.805 |
1.028-7.654 |
0.044* |
|
EST |
0.559 |
0.202-1.552 |
0.265 |
|
|
|
|
Pancreatic duct opacification |
2.534 |
1.232-5.214 |
0.012* |
3.463 |
1.530-7.837 |
0.003** |
|
Nasobiliary drainage |
0.479 |
0.229-1.001 |
0.050 |
0.398 |
0.079-2.015 |
0.266 |
|
PEP: Post-ERCP pancreatitis; ERCP: Endoscopic retrograde cholangiopancreatography; SOD: Sphincter of Oddi dysfunction; EST: Endoscopic sphincterotomy. *p <0.05, **p <0.01, ***p <0.001. |
||||||
The scoring model was applied to each of the 375 patients in the study, and ROC curves were plotted. The area under the ROC curve was 0.764, and the optimal cuto-ff value was determined to be 1.5 points (Figure 1).
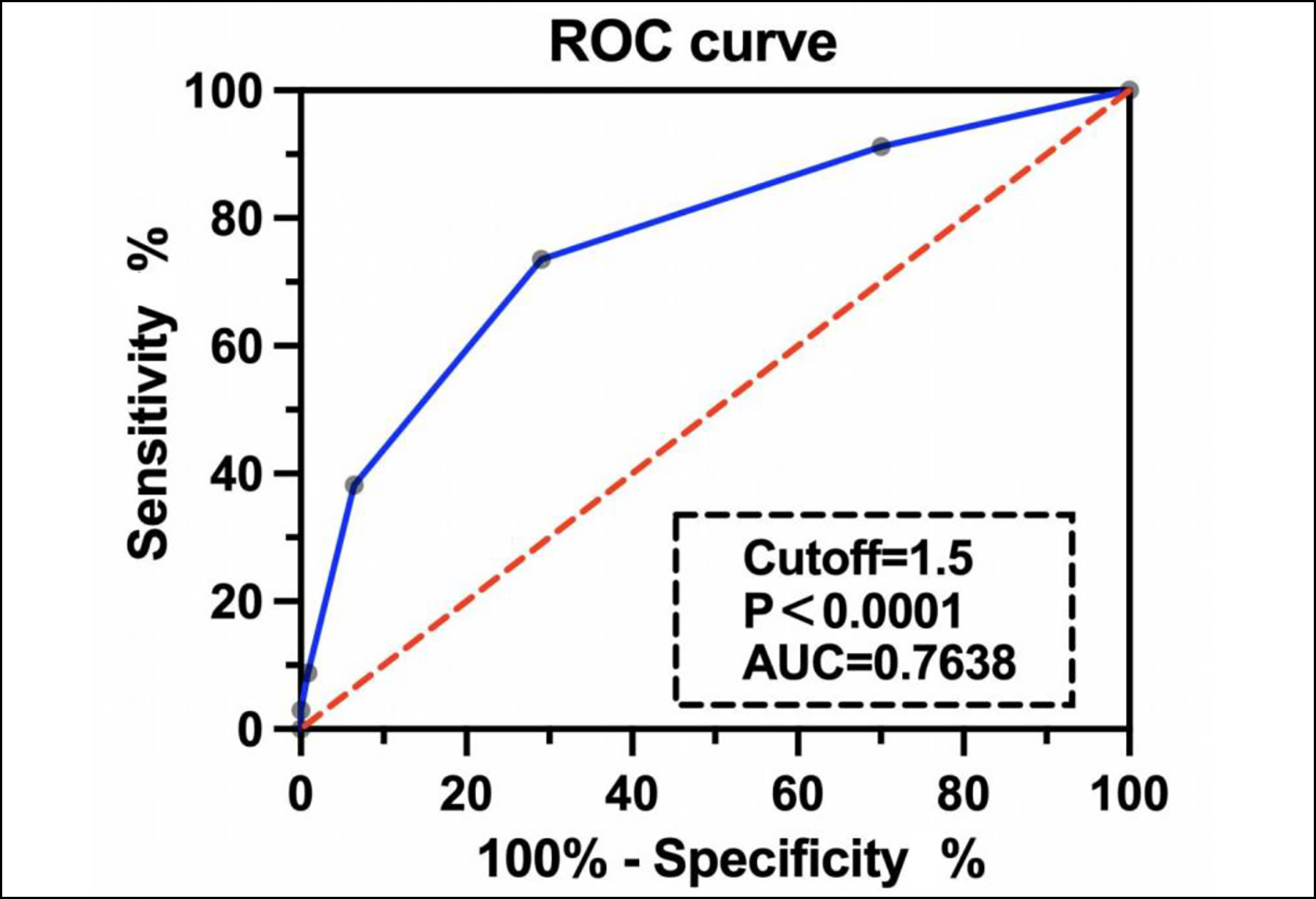 Figure 1: The sensitivity and specificity of the PEP risk model.
Figure 1: The sensitivity and specificity of the PEP risk model.
DISCUSSION
ERCP is a widely used diagnostic and therapeutic technique for liver, gallbladder, and pancreatic diseases. However, it is characterised by high technical difficulty and carries inherent risks. Complications following ERCP, such as PEP, are prevalent and serious due to the complex and diverse anatomy of the biliary system. In this study, the observed frequency of PEP at 9.07% aligned with reported incidences in the literature, emphasising its consistent prevalence as a significant complication following ERCP.1 While the exact pathogenesis of PEP remains unclear, it is commonly associated with factors such as post-examination or post-treatment pancreatic congestion, which may impact pancreatic juice viscosity and lead to pancreatic duct obstruction. Further investigation into the multifaceted mechanisms contributing to the onset of PEP is warranted to improve the understanding and prevention of this complication.
PEP can be attributed to various risk factors, including patient-related and procedure-related factors. Patient-related factors are currently believed to contribute to PEP include being female, age younger than 60 years, extrahepatic bile duct stenosis, duodenal diverticulum, normal serum bilirubin, suspected SOD, history of pancreatitis, hypertension, diabetes, biliary tract disease, previous ampullary surgery, and anatomical abnormalities. Procedure-related factors that are currently considered relevant to PEP include sphincterotomy, difficult cannulation, excessive cannulation attempts, wire insertion into the pancreatic duct, pancreatic duct opacification, high concentration and volume of contrast agent, pancreatic stent placement, as well as the clinician's clinical experience and technical proficiency. In this study, the univariate analysis identified female, pancreatic duct opacification, SOD, difficult cannulation, operative time ≥45 minutes, and biliary stent placement as significant risk factors for PEP (p<0.05), while other factors were not statistically significant. Logistic regression analysis targeting these risk factors found that female, pancreatic duct opacification, difficult cannulation, SOD, and operative time ≥45 minutes were independent risk factors for PEP (p<0.05).
Gender has been identified as a significant factor in the development of PEP.6 Women may be more susceptible to certain psychological factors and stress responses, leading to increased pancreatic secretions and exacerbation of pancreatic damage, even with minor injury during ERCP.7 Furthermore, some studies have found that women have a higher incidence of sphincter of Oddi dysfunction (SOD), which increases the risk of PEP.8 However, large-scale prospective studies have shown no significant difference in PEP incidence between genders, and a retrospective study of 2,715 patients found no association between gender or SOD and PEP occurrence.9 In contrast, this study, which included 375 patients with a similar distribution of men and women, found that the incidence of PEP in women was significantly higher than in men (12.97% vs. 5.26%). Additionally, the results of the multivariate logistic regression analysis confirmed that female gender is an independent risk factors for PEP.
Difficult cannulation, defined as an insertion time of ≥ 10 minutes or ≥5 insertion attempts, has been established as an independent risk factor for PEP by Wang et al.10 Repeated attempts during ERCP can cause mechanical stimulation and injury to the papilla, leading to congestion, oedema, and spasm of the Oddi sphincter. This impairment of pancreatic drainage ultimately triggers the occurrence of PEP.11 In this study, patients were categorised based on an operation time of 45 minutes, with 64 cases having an operation time of ≥ 45 minutes, and a PEP incidence of 20.31%. The results of the logistic regression analysis demonstrated a significant association between an operation time of ≥45 minutes and PEP (p<0.05), highlighting it as an independent risk factor for PEP.
Pancreatography has been established as a risk factor for PEP.12 The dose of contrast medium administered into the pancreatic duct has a positive correlation with the incidence of PEP.11 Furthermore, the presence of residual contrast medium within the pancreatic duct and the experience of sustained abdominal pain for 3 hours after the operation are critical risk factors for severe PEP.13 Upon contrast medium injection into the pancreatic duct, it creates a high-pressure environment, which can cause the backflow of pancreatic juice into the pancreatic parenchyma. A positive feedback mechanism triggers the activation of pancreatic enzymes, leading to the destruction of pancreatic tissue. Additionally, the high-pressure environment within the duct can hinder pancreatic enzyme secretion, ultimately resulting in the accumulation of zymogen granules in digestive cells and premature activation of pancreatic enzymes. This sequence of events ultimately culminates in pancreatitis.10 George et al. discovered that the risk of PEP was generally similar among patients who received contrast media with different osmotic pressures.14 This observation implied that during the operation, the injection of contrast medium should proceed at a slow pace to avoid causing damage to the pancreatic duct hydrostatic pressure.
Oddi sphincter dysfunction (SOD) is a pathological condition characterised by impaired function of the sphincter of Oddi. This dysfunction leads to abnormal flow of bile and pancreatic juice at the junction of the biliary, pancreatic, and duodenal ampulla. Consequently, it causes a variety of symptoms, such as upper abdominal pain, biliary colic, nausea, and vomiting. SOD plays a critical role in the development of PEP, as it can hinder the outflow of pancreatic fluid, resulting in the accumulation of fluid within the duct and subsequent injury due to hydrostatic pressure.15 In this study, irrespective of whether the ERCP procedure was performed for diagnostic, sphincter pressure measurement, or therapeutic purposes, a significantly higher incidence of PEP was observed in patients suspected of having SOD, reaching 42.86% (3/7). Logistic regression analysis of the risk factors also confirmed a significant association between SOD and the occurrence of PEP (p <0.05).
A scoring system was developed aimed at guiding the prevention of PEP. The probability of PEP increased significantly when a patient's score exceeded 1.5. In such cases, it is important to implement intraoperative and postoperative preventive measures in order to reduce the incidence of PEP.
To reduce the occurrence of PEP, clinicians can employ preventive measures from three aspects; clarifying treatment indication, pharmacological prevention, and technical prevention. In cases of diagnostic ERCP, it is advisable to consider safe and effective alternatives such as magnetic resonance cholangiopancreatography (MRCP) or endoscopic ultrasonography (EUS) as the primary options. For patients requiring therapeutic intervention, it is crucial for endoscopists to have a comprehensive understanding of the patient's risk factors and carefully evaluate the potential benefits and risks to develop appropriate treatment plans and preventive measures. Pharmacological prevention can be achieved through the use of selective and non-selective nonsteroidal anti-inflammatory drugs (NSAIDs) as well as somatostatin and its analogues, which have been shown to be effective.16 In terms of technical prevention, the placement of a pancreatic stent is an effective method for maintaining the pancreatic duct patency and relieving pancreatic duct hypertension.17 Additionally, procedures such as endoscopic nasobiliary drainage (ENBD) and biliary stent drainage can effectively drain bile, reduce biliary pressure, prevent bile reflux into the pancreatic duct, and alleviate pancreatic duct pressure caused by residual stones and papillary oedema.18
This study has several limitations. Firstly, it is important to note that this study is retrospective in nature, which means that the data may not be as comprehensive and accurate as those obtained from a prospective cohort study. Secondly, this study was conducted at a single-centre with a relatively small sample size, which introduces inherent limitations and potential errors. However, despite these limitations, the study provided significant insights into the risk factors associated with post-ERCP pancreatitis. Furthermore, the development of a risk assessment model provides valuable guidance for clinicians in the prevention of PEP. By custo-mising interventions for high-risk individuals, optimising pharmacological prophylaxis, and refining procedural techni-ques, the occurrence and severity of this prevalent and potentially life-threatening complication can be effectively decreased.
CONCLUSION
The identified independent risk factors include female, pancreatic duct opacification, difficult cannulation, SOD, and operative time ≥45 minutes. Patients with scores less than 1.5 points had a lower incidence of PEP, while those with scores greater than 1.5 points had a higher incidence. When a patient meets any two conditions from being female, pancreatic duct opacification, difficult cannulation, operative time ≥45 minutes, and SOD, clinicians should take proactive preventive measures during the perioperative period to reduce the incidence of PEP.
ETHICAL APPROVAL:
This study was approved by the ethics committee of the Affiliated Hospital 2 of Nantong University on January 1, 2022 (Approval Number: 2022KT256).
PATIENTS’ CONSENT:
Written informed consent was taken from all patients.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
CZ: Conception and design, provision of study materials or patients, and manuscript writing.
TD: Collection and assembly of data.
JQ: Manuscript writing.
ZG: Significantly revised the manuscript.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, et al. Adverse events associated with ERCP. ASGE Standards of Practice Committee; Gastrointest Endosc 2017; 85(1):32-47. doi: 10.1016/j.gie.2016.06.051.
- El Nakeeb A, El Hanafy E, Salah T, Atef E, Hamed H, Sultan AM, et al. Post-endoscopic retrograde cholangio-pancreatography pancreatitis: Risk factors and predictors of severity. World J Gastrointest Endosc 2016; 8(19): 709-15. doi: 10.4253/wjge.v8.i19.709.
- Kochar B, Akshintala VS, Afghani E, Elmunzer BJ, Kim KJ, Lennon AM, et al. Incidence, severity, and mortality of post-ERCP pancreatitis: A systematic review by using randomized, controlled trials. Gastrointest Endosc 2015; 81(1):143-9. doi: 10.1016/j.gie.2014.06.045.
- Kubiliun NM, Elmunzer BJ. Preventing pancreatitis after endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am 2013; 23(4):769-86. doi:10.1016/j.giec.2013.06.003.
- Ribeiro IB, do Monte Junior ES, Miranda Neto AA, Proença IM, de Moura DTH, Minata MK, et al. Pancreatitis after endoscopic retrograde cholangiopancreatography: A narrative review. World J Gastroenterol 2021; 27(20): 2495-506. doi: 10.3748/wjg.v27.i20.2495.
- Freeman ML. Post-ERCP pancreatitis: Patient and technique-related risk factors. JOP J Pancreas 2002; 3(6): 169-76.
- Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal JF, Montagner A, et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 2020; 63(3): 453-61. doi: 10.1007/s00125-019-05040-3.
- Ding X, Zhang F, Wang Y. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surg J R Coll Surg Edinb Irel 2015; 13(4):218-29. doi:10.1016/ j.surge.2014.11.005.
- Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, et al. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol 2014; 27(1):65-72.
- Wang J, Su J, Lu Y, Zhou H, Gong B. A randomized control study to investigate the application of Ulinastatin-containing contrast medium to prevent post-ERCP pancreatitis. Hepatogastroenterology 2014; 61(136): 2391-4.
- Cheon YK, Cho KB, Watkins JL, McHenry L, Fogel EL, Sherman S, et al. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc 2007; 65(3):385-93. doi: 10.1016/j.gie.2006.10.021.
- Shimamura T, Miyahara K, Takamori A, Hidaka H, Ito Y, Fujimoto S, et al. Risk factors for post-endoscopic retrograde pancreatography pancreatitis: A retrospective chart review in a regional hospital in Japan. Digestion 2020; 101(5):557-62. doi: 10.1159/000501309.
- Matsubara H, Urano F, Kinoshita Y, Okamura S, Kawashima H, Goto H, et al. Analysis of the risk factors for severity in post endoscopic retrograde cholangiopancreatography pancreatitis: The indication of prophylactic treatments. World J Gastrointest Endosc 2017; 9(4):189-95. doi: 10.4253/wjge.v9.i4.189.
- George S, Kulkarni AA, Stevens G, Forsmark CE, Draganov P. Role of osmolality of contrast media in the development of post-ERCP pancreatitis: A metanalysis. Dig Dis Sci 2004; 49(3):503-8. doi:10.1023/b:ddas.0000020511.98230.20.
- Ergin E, Oruç N, Ersöz G, Tekeşin O, Özütemiz Ö. Prognosis and risk factors of ERCP pancreatitis in elderly. Sci Rep 2021; 11(1):15930. doi:10.1038/s41598-021-95484-8.
- Geng C, Li X, Li Y, Song S, Wang C. Nonsteroidal anti-inflammatory drugs alleviate severity of post-endoscopic retrograde cholangiopancreatography pancreatitis by inhibiting inflammation and reducing apoptosis. J Gastro-enterol Hepatol 2020; 35(5):896-904. doi:10.1111/jgh. 15012.
- Mine T, Morizane T, Kawaguchi Y, Akashi R, Hanada K, Ito T, et al. Clinical practice guideline for post-ERCP pancreatitis. J Gastroenterol 2017; 52(9):1013-22. doi: 10.1007/s00 535-017-1359-5.
- Okuno M, Iwata K, Mukai T, Iwasa Y, Ogiso T, Sasaki Y, et al. Endoscopic nasobiliary drainage tube placement through a periampullary perforation for management of intestinal leak and necrotizing pancreatitis. VideoGIE 2022; 8(2):75-7. doi: 10.1016/j.vgie.2022.09.004.